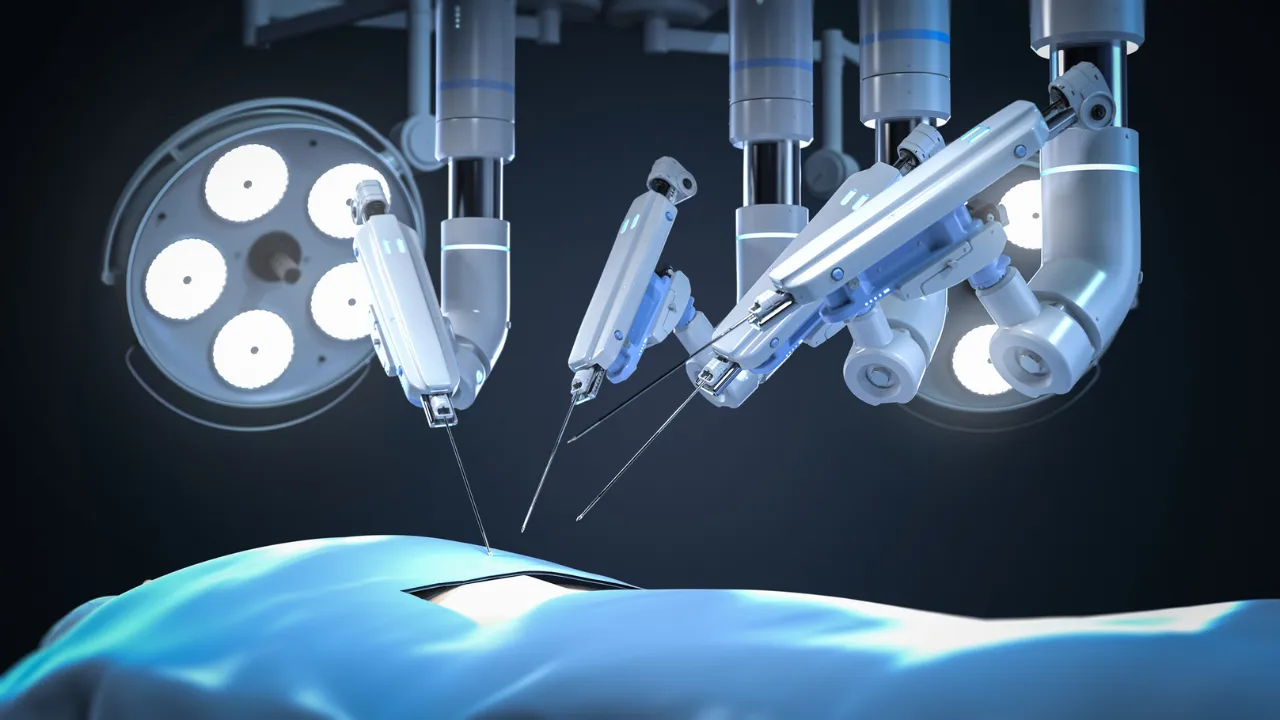
EndoQuest Robotics Performs World’s First Fully Robotic Endoscopic Submucosal Dissection by a Gastroenterologist
27 October 2025 | Interaction | By editor@rbnpress.com
EndoQuest Robotics CEO Eduardo Fonseca shares insights on pioneering the first fully robotic endoscopic submucosal dissection and the future of minimally invasive GI surgery.
In an exclusive interview with Robotics Business News, Eduardo Fonseca, CEO of EndoQuest Robotics and XCath, discusses how the EndoQuest Endoluminal Surgical (ELS) System is transforming gastrointestinal procedures. The platform enables gastroenterologists to perform fully robotic endoscopic submucosal dissections with precision and efficiency, streamlining workflows, reducing procedural complexity, and expanding access to minimally invasive therapies. Fonseca also highlights the PARADIGM trial, training protocols, and the company’s vision for broader adoption and commercialization.
What distinguishes this procedure as the world’s first fully robotic endoscopic submucosal dissection by a gastroenterologist—what parts of the workflow were robotic vs manual?
The EndoQuest Endoluminal Surgical (ELS) System enabled the entire resection and closure phases of the ESD procedure to be performed using robotic instruments, a robotic camera, and a robotic overtube (EndoDrive™), each entirely controlled by the physician at the Physician Console using hand controllers and foot pedals.
Before the ELS System, robotic endoscopic submucosal dissections (ESDs) performed by gastroenterologists have utilized hybrid robotic platforms, which aim to address some of the challenges faced by therapeutic endoscopists such as providing countertension. However, these platforms interface with conventional manual endoscopes, require a second physician at the bedside to operate the endoscope, and only partially address the limitations of therapeutic endoscopy. The ELS System is the only fully robotic, flexible endoluminal platform in late-stage development, uniquely focused on delivering generalized therapeutic capabilities for endoluminal surgery.
How did you select the site and endoscopist (Dr. Norio Fukami) for performing this landmark case, and what training or credentialing was required?
As a world-renowned expert in ESD and other advanced endoluminal and pancreaticobiliary techniques, and with one of the highest ESD volumes in the U.S., Dr. Fukami was a natural fit for a gastroenterologist to pioneer use of the ELS System in the PARADIGM Trial.
Prior to performing this case, Dr. Fukami completed the IDE-approved EndoQuest Training Program on use of the ELS System required for all physicians participating in the PARADIGM Trial. Prior to hands-on training on the robotic system, Dr. Fukami first trained on the EndoQuest digital twin simulator to achieve initial basic system familiarization and skills development.
What are the primary and secondary endpoints for the PARADIGM trial, and how will you judge procedural success, safety, and long-term outcomes?
The primary endpoints for the PARADIGM Trial are en bloc resection rate (efficacy) and ESD-related complication-free rate (safety). Secondary effectiveness endpoints include R0 resection rate and conversion-free rate. Additional secondary endpoints include readmission rate, length of stay, postoperative complication-free rate, estimated blood loss, ESD procedure time, and resection speed. Further details on the study data to be collected are provided on Clinicaltrials.gov.
What is your plan for expanding this approach to gastroenterologists more broadly (versus colorectal surgeons), and how will you manage the learning curve?
We believe that a safe and successful expansion of the ELS System will depend primarily on comprehensive training, proctoring, and procedural support as physicians navigate the learning curve – similar to the introduction of other transformative medical technologies. As clinical experience grows, EndoQuest plans to formalize a structured training curriculum building on the foundation of the program developed for the IDE trial.
Our initial focus includes both surgeons and gastroenterologists who are already performing advanced endoscopic procedures or who have completed, or are currently enrolled in, Advanced Endoscopy Fellowships. While expert endoscopists such as Dr. Fukami represent ideal participants for our initial clinical trial, the ELS System is ultimately designed to broaden access to complex therapeutic endoscopy. We believe our platform truly enables the gastroenterologist without significant advanced endoscopy experience to accelerate their learning curve and transform their capabilities. This trajectory parallels how robotic surgery transformed urology in the early 2000s – enabling widespread adoption of minimally invasive prostatectomy by lowering technical barriers associated with traditional laparoscopy. Similarly, we anticipate that the ELS System will help expand minimally invasive therapeutic options for patients by equipping a broader group of gastroenterologists to perform advanced procedures safely and effectively.
How do you envision this technology shifting procedural workflows, OR or endoscopy suite requirements, and the infrastructure needed in GI clinics/hospitals?
We anticipate that the ELS System will significantly streamline procedural workflows by enabling ESD to be performed in substantially less time than with conventional endoscopic techniques – and considerably faster than colectomies. This reduction in procedure time may translate to greater OR and endoscopy suite efficiency at institutions offering these procedures. While robotic ESD requires a brief additional setup period to position the robotic platform and prepare instrumentation, the total procedure duration is expected to remain shorter overall, as the dissection phase is completed far more efficiently. This represents a meaningful tradeoff between setup and procedural speed, especially as clinical staff achieve proficiency in setup. Because robotic colectomies are already common in the U.S., many facilities are familiar with traditional robotic workflows and equipment integration. By enabling ESD to be performed more efficiently and reproducibly, the ELS System may allow more patients to benefit from a less invasive, organ-sparing alternative to colectomy that can reduce complications, preserve anatomy, and support faster recovery.
The ELS System has been designed for flexible deployment in small operating rooms and endoscopy suites, and future iterations following De Novo authorization are expected to further enhance this adaptability. In terms of staffing and operational needs, the ELS System integrates seamlessly into current team structures, requiring one physician, one bedside assistant (such as a sterile tech or endoscopy tech), and one circulator – consistent with or fewer than current requirements for ESD or colectomy. The primary new consideration will be ensuring that facilities possess the appropriate infrastructure for cleaning and sterilizing complex surgical instruments, beyond what is typically required for standard flexible endoscopes.
Ultimately, the ELS System is positioned to redefine the endoscopy suite and expand patient access to minimally invasive therapeutic procedures, while improving clinical efficiency, procedural throughput, and overall resource utilization within hospitals and endoscopy centers.
Assuming positive trial results, what is your regulatory and commercialization pathway—e.g. De Novo, FDA approval, reimbursement, and adoption strategy?
Following completion of the PARADIGM trial, EndoQuest Robotics plans to submit a De Novo request to the FDA for authorization to market the ELS System in the United States. In parallel, the company is advancing additional clinical procedures and next-generation platform developments to broaden the system’s capabilities. After initial De Novo authorization, EndoQuest plans to pursue expanded indications to upper GI, bariatrics, reflux, ERCP and a broad range of other endoluminal applications, which are expected to follow the 510(k) regulatory pathway.
From a reimbursement perspective, the newly established CPT code for ESD is scheduled to take effect in January 2027, positioning EndoQuest to align commercialization with the introduction of established reimbursement for this procedure. This follows growing recognition of advanced endoluminal therapies, including the new CPT code for endoscopic sleeve gastroplasty (ESG) effective January 2026, reflecting expanding payer support for minimally invasive endoscopic interventions.
EndoQuest’s commercialization strategy will focus on a targeted launch with high-volume centers and early adopters experienced in advanced endoscopy and robotic innovation, supported by a structured training and proctoring program to ensure safe, effective adoption across the field.